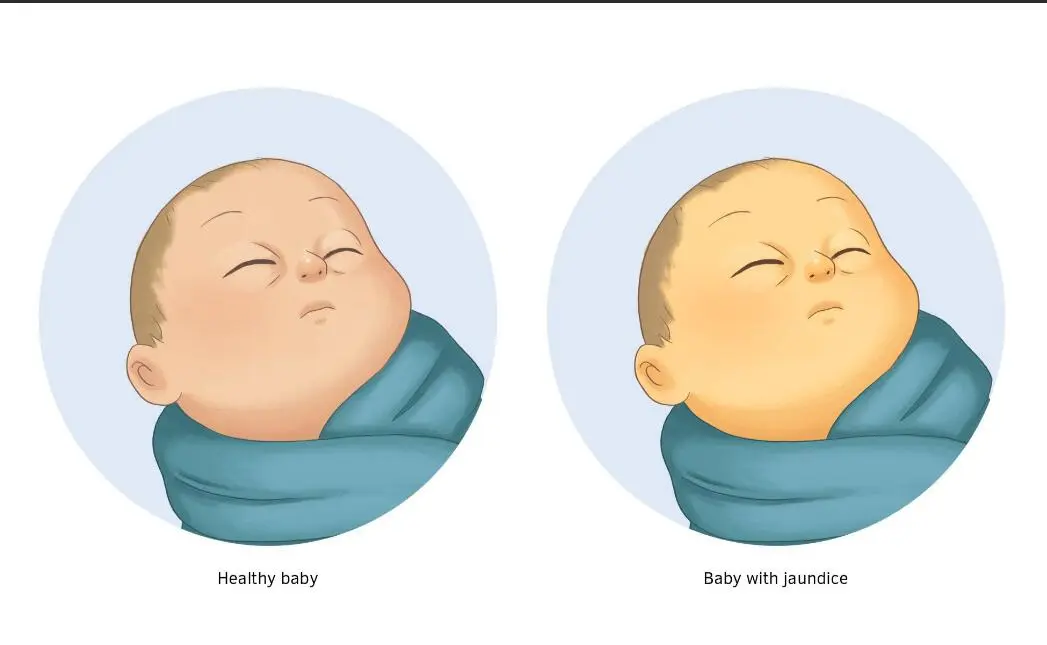
Neonatal jaundice is a condition characterized by yellowing of the skin, mucous membranes, and sclerae due to elevated levels of bilirubin in the blood. Traditionally, neonatal jaundice can be classified as physiological or pathological, but it cannot be solely differentiated based on serum bilirubin levels.
Neonatal jaundice is the most common clinical symptom in the neonatal period. Physiological jaundice tends to resolve on its own, and the duration of jaundice is longer in preterm infants. Pathological jaundice has complex etiology and severe jaundice can result in brain damage.
Symptoms of Neonatal Jaundice:
Yellowing of the skin and eyes: The most noticeable symptom of neonatal jaundice is the yellow discoloration of the skin and the whites of the eyes. This yellowing typically starts from the head and face and spreads downwards.
Pale stools: Infants with jaundice may have pale or clay-colored stools instead of the normal yellowish-brown color. This is due to the excess bilirubin being excreted through the stool.
Dark urine: Along with pale stools, newborns with jaundice may have dark-colored urine. The elevated bilirubin levels in the blood can cause the urine to appear darker than usual.
Poor feeding or lethargy: Some infants with severe jaundice may exhibit feeding difficulties or appear excessively sleepy or lethargic. This can be a sign of more severe jaundice requiring immediate medical attention.
Physiological Jaundice
Infants with physiological jaundice have good mental response, normal sleep and feeding patterns, and normal bowel and bladder movements. It is a normal physiological phenomenon in newborns.
The diagnosis of physiological jaundice in newborns should meet the following criteria:
- Term infants (gestational age ≥37 weeks) develop jaundice 2-3 days after birth, peak at 4-5 days, and resolve within 5-7 days, with a maximum duration of 2 weeks.
- Preterm infants (gestational age <37 weeks) develop jaundice 3-5 days after birth, peak at 5-7 days, resolve within 7-9 days, and can be delayed up to 3-4 weeks.
Serum total bilirubin levels have not exceeded the 95th percentile on the hour-specific bilirubin nomogram for newborns, or have not reached the phototherapy intervention criteria for corresponding postnatal age, gestational age, and associated risk factors.
Pathological Jaundice
Common causes of pathological jaundice include hemolytic jaundice (due to maternal-fetal blood type incompatibility), breastfeeding jaundice (seen in some breastfed newborns), infectious jaundice (including intrauterine and postnatal infections), and obstructive jaundice (congenital biliary malformations).
Any of the following criteria indicates pathological jaundice, which requires prompt medical attention and further investigation of the underlying cause:
- Early onset, with jaundice appearing within 24 hours after birth.
- Severe, with serum total bilirubin levels exceeding the 95th percentile on the hour-specific bilirubin nomogram for newborns, or meeting the phototherapy intervention criteria for corresponding postnatal age, gestational age, and associated risk factors.
- Rapidly increasing severity, with a daily rise in total bilirubin levels greater than 5mg/dl.
- Prolonged duration, lasting more than 2 weeks in term infants or more than 4 weeks in preterm infants.
- Recurrence of jaundice after initial resolution.
Misconceptions
Neonatal jaundice can be ignored as it will resolve on its own.
While physiological jaundice in newborns generally resolves on its own, pathological jaundice has a complex underlying cause and can persist for a longer duration. If the underlying cause is not identified and treated appropriately, jaundice can reappear after it initially resolves.