Every 20 seconds, one person around the world undergoes amputation due to diabetes. The annual mortality rate for diabetic foot ulcers is as high as 11%, while amputated patients face an even higher mortality rate of 22%.
Many diabetes patients are unaware that a small foot ulcer can lead to major amputation or even death.
Diabetic foot problems don't occur suddenly. If your body shows any of the following 14 signals, it's highly likely that diabetic foot has arrived.
10 Signals of Lower Extremity Vascular Disease
Lower extremity vascular disease caused by diabetes reduces blood flow to the legs, resulting in tissue hypoxia and insufficient nutrient supply. This can lead to coldness, pain, and intermittent claudication in the legs. Severe cases can cause diabetic foot ulcers and gangrene.
Leg pain
Lower extremity vascular disease can cause leg pain, which can be continuous or intermittent, and the severity can vary. The pain is often located in the distal part of the legs and is usually symmetrical.
Numbness in the legs
Lower extremity vascular disease can also cause numbness in the legs, resulting in abnormal sensations such as tingling or crawling sensations. Numbness is often felt in the distal part of the legs and can significantly affect normal limb function.
Cold feet
Poor blood circulation caused by lower extremity vascular disease can make the feet feel cold, especially when one foot feels much colder than the other. This sensation is more pronounced in winter and can lead to tissue necrosis in severe cases.
Intermittent claudication
Due to reduced blood supply caused by lower extremity vascular disease, patients may experience intermittent claudication after walking for a certain period. This is characterized by difficulty in walking and significant pain, which subsides after rest.
Muscle atrophy in the legs
Lower extremity vascular disease can lead to muscle atrophy in the legs, resulting in reduced muscle volume and strength. This not only affects daily activities but can also cause patients to lose their ability to walk.
Foot ulcers
Poor blood circulation in the feet caused by lower extremity vascular disease makes patients prone to foot ulcers. Initially, the skin may appear red and swollen, but in severe cases, it can progress to skin breakdown and infection.
Weakened dorsalis pedis pulse
Lower extremity vascular disease can cause arterial sclerosis and weaken the dorsalis pedis pulse. In severe cases, the pulse may disappear, affecting blood supply and leading to tissue necrosis.
Leg swelling
Lower extremity vascular disease can obstruct lymphatic drainage, leading to leg swelling. Swelling is often observed in the distal part of the legs and can extend to the entire limb in severe cases.
Changes in leg skin
Loss of hair on the legs, skin pigmentation, or pale skin in the legs are all manifestations of vascular dysfunction.
Changes in toenail appearance
If the toenails are not smooth, have uneven surfaces, lack luster, or appear dark gray, it indicates poor blood supply to the distal part of the foot.
4 Signals of Lower Extremity Neuropathy
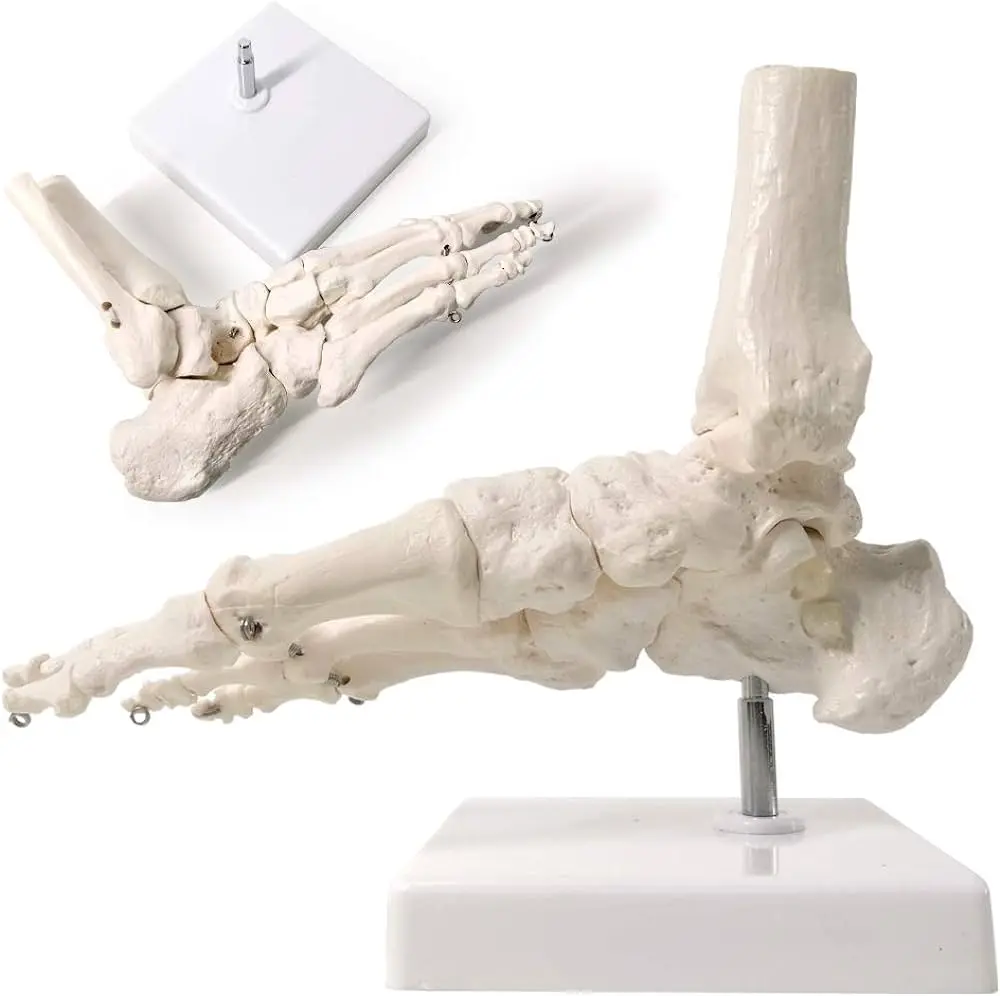
Foot deformities
Motor neuropathy affects the tension of foot muscles, causing muscle atrophy and changing the weight-bearing position of the foot. This can result in foot deformities such as claw toes or hammer toes.
Loss of protective sensation
Nerve damage leads to a loss of protective sensation, making the foot less responsive to external pressures, foreign objects, or temperature changes. This increases the likelihood of injury and ulcer formation.
Abnormal sensation in the legs
Patients may experience tingling, burning, or numbness in the distal part of the legs, resembling the sensation of wearing socks filled with cotton.
Dry and cracked foot skin
Autonomic neuropathy in diabetes reduces sweat gland function, leading to dry and cracked foot skin, which can easily become infected.
In addition to the 14 signals of lower extremity vascular and neuropathic diseases, we must not overlook minor foot problems such as calluses, corns, ingrown toenails, itchy skin, or fungal infections. Seeking professional medical help in a timely manner is crucial.
Take Foot Care Seriously as a Diabetes Patient: Preventing Problems from Escalating!